The endotracheal tube (ETT) is a vital medical device that plays a crucial role in airway management. It is widely used in anesthesia, intensive care, and emergency situations to maintain patient breathing and prevent airway obstruction. In many cases, endotracheal intubation is essential for patients experiencing acute respiratory distress, cardiopulmonary arrest, or decreased consciousness.
The endotracheal tube allows healthcare professionals to deliver oxygen efficiently while also enabling mechanical ventilation when necessary to support lung function. In surgical settings, it is an integral part of general anesthesia, ensuring airway patency and preventing aspiration of gastric contents into the lungs, thereby enhancing patient safety.
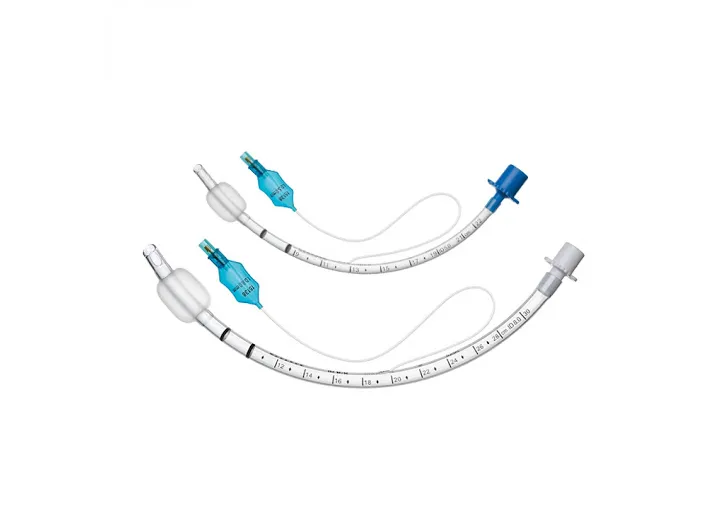
Endotracheal tubes come in various sizes and designs to accommodate different age groups and medical conditions. Some models feature a cuff that inflates to prevent air leakage and help secure the tube in place within the trachea. Others are cuffless, typically used in neonates and young children with more sensitive airways.
Ultimately, the endotracheal tube is one of the most critical medical instruments, playing a key role in saving lives. Proper use requires specialized knowledge and skill, as adherence to clinical guidelines in intubation, post-intubation care, and tube selection significantly impacts treatment success and minimizes potential complications.
Endotracheal Tube
Structure and Components of the Endotracheal Tube
The endotracheal tube is a flexible plastic tube, typically made of polyvinyl chloride (PVC). It consists of various components, each serving a specific function:
Tube Body: The main part of the tube that delivers air or anesthetic gases to the lungs.
Cuff: A balloon near the distal end of the tube that inflates to secure the tube in place, preventing air leakage and aspiration of secretions into the lungs.
Pilot Balloon: A small external balloon that indicates the status of the cuff; by palpating it, clinicians can determine whether the cuff is inflated or deflated.
Radiopaque Line: A strip along the tube that is visible in radiographic images, assisting physicians in confirming the tube’s placement within the body.
Types of Endotracheal Tubes
Endotracheal tubes are designed in various types to accommodate different patient needs and clinical situations:
Cuffless Endotracheal Tube: These tubes lack an inflatable cuff and are primarily used in children under eight years old. In younger patients, the natural tracheal structure helps secure the tube, reducing the risk of tracheal tissue damage.
Cuffed Endotracheal Tube: Equipped with an inflatable cuff that stabilizes the tube in the trachea, prevents air leakage, and blocks secretions from entering the lungs. This type is commonly used in adults, long-duration surgeries, and cases requiring mechanical ventilation.
Reinforced (Armored) Endotracheal Tube: These tubes contain a metal spiral reinforcement that prevents kinking or obstruction. They are useful in surgeries where patient or head positioning may change frequently.
Double-Lumen Endotracheal Tube: Featuring two separate channels, these tubes allow independent ventilation of each lung. They are commonly used in thoracic surgeries or procedures requiring lung isolation.
RAE (Ring-Adair-Elwyn) Endotracheal Tube: Designed with a preformed bend that directs the tube away from the surgical field, making it ideal for oral and maxillofacial surgeries.

Endotracheal Tube
Endotracheal Intubation Process
Intubation is the procedure of inserting an endotracheal tube through the mouth or nose into the trachea to maintain an open airway. This process requires skill and experience and is usually performed by an anesthesiologist or an emergency physician.
General Steps of Intubation:
Preparation: Ensuring all necessary equipment is available, checking the functionality of the laryngoscope, and selecting the appropriate tube size based on the patient’s age and condition.
Patient Positioning: Placing the patient in an optimal position (usually supine with the head extended) for better airway access.
Anesthesia and Sedation: Administering anesthetic and muscle relaxant medications to minimize pain and prevent involuntary reactions.
Tube Insertion: Using a laryngoscope to visualize the vocal cords and guide the endotracheal tube through them into the trachea.
Tube Placement Confirmation: Checking breath sounds in both lungs, observing chest movement, and, if needed, using capnography or radiographic imaging to confirm correct tube placement.
Tube Stabilization: Inflating the cuff (if present) and securing the tube to the patient’s lips or face with tape or specialized holders.
Post-Intubation Care
Proper post-intubation care is essential to prevent complications and ensure effective tube function:
Regular Tube Position Checks: Ensuring the tube remains in place and preventing accidental displacement or removal.
Air Humidification: Using humidification systems to prevent tracheal and lung mucosa from drying out.
Suctioning Secretions: Regularly clearing accumulated secretions in the tube and airway to prevent blockage and infections.
Cuff Pressure Monitoring: Ensuring proper cuff inflation to prevent airway leaks and tracheal wall damage. Excessive pressure may cause tracheal ischemia, while insufficient pressure can lead to air leakage and aspiration risk.
Infection Prevention: Endotracheal tubes can contribute to hospital-acquired infections, such as ventilator-associated pneumonia (VAP). Adhering to strict hygiene protocols, regular suctioning, and using disinfectant solutions are crucial.
Duration of Intubation: If prolonged mechanical ventilation is required, transitioning to an alternative method like tracheostomy should be considered to reduce the risk of tracheal injury.
Extubation (Tube Removal): Once the patient regains spontaneous breathing ability and maintains stable conditions, the tube is removed. This process requires careful assessment of respiratory strength, blood oxygen levels, and airway protection capability.
Conclusion: Understanding Endotracheal Tubes
The endotracheal tube is a critical medical device used for airway management in surgeries, intensive care, and emergency situations. Selecting the appropriate type of tube, performing intubation correctly, and providing post-procedural care directly impact patient health and recovery. Adhering to medical standards and hygiene protocols can reduce complications and improve treatment outcomes.
What are your thoughts on this introduction to endotracheal tubes? If you have any feedback, we would be delighted to hear from you at Salamat Gostar Nano Daroo.
If you’re interested, you can visit our website to learn more about this product. If you have any questions or need guidance, the Salamat Gostar Nano Daroo support team is available during business hours. For faster communication, feel free to contact us via WhatsApp.

